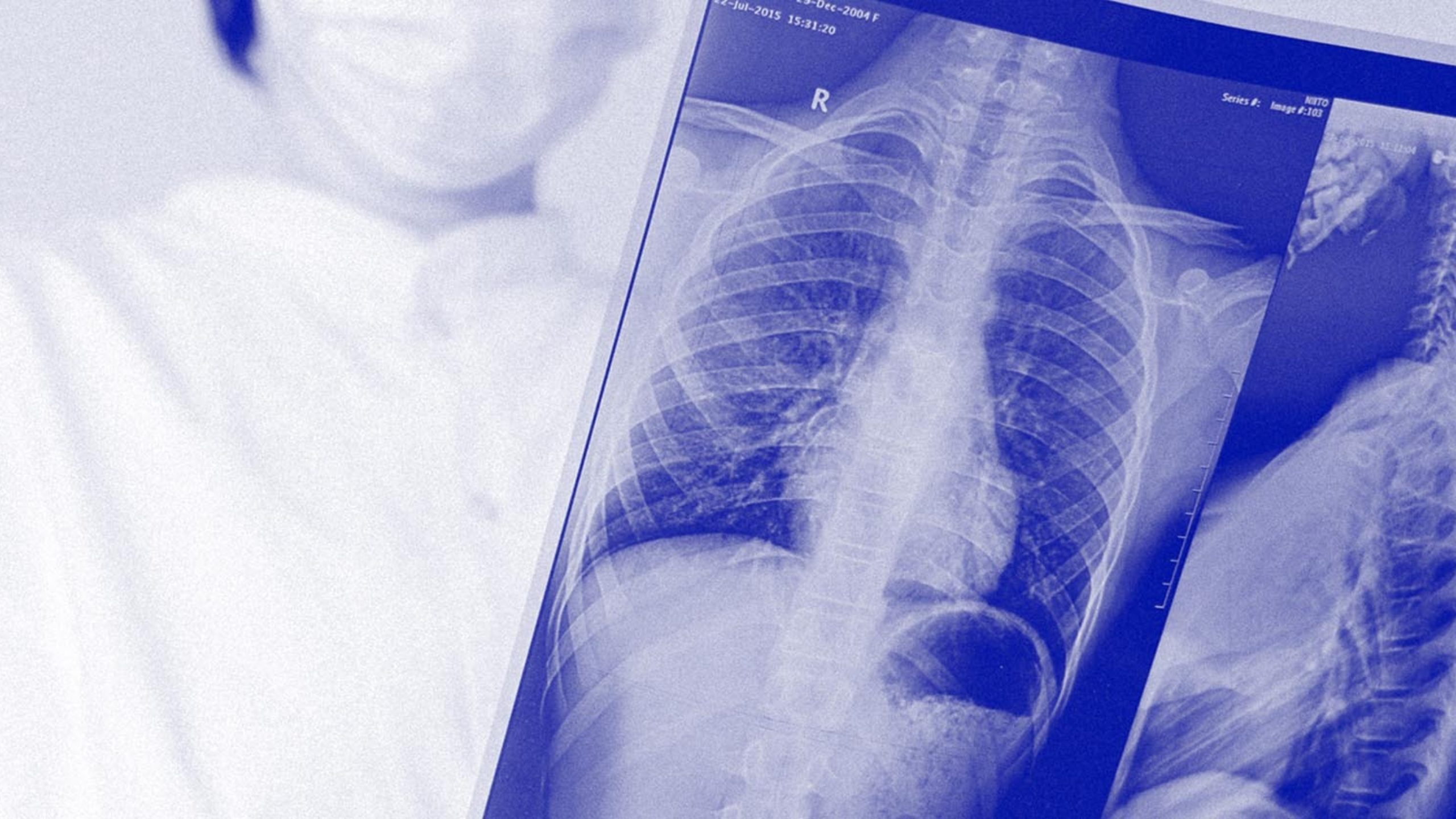
Let's Fight
Lung Disease
Almost 1 in 3 Australians are impacted by lung disease and anyone can be at risk. Symptoms may progress slowly before advancing to a potentially life-threatening state. From airway diseases to lung tissue and circulation disease, there are over 30 types of lung disease.
Helping people breathe easier
Lung disease can significantly impact people’s enjoyment of life, hindering their ability to be active and productive.
Previously, lung disease carried the stigma that only those who have been smokers are affected, however, this is not the case. Through advancements in research, we can improve the quality of life for those impacted by lung disease by developing better treatments, interventions, and early diagnosis opportunities.

Recent projects
Helping workers breath easier with whole lung lavage
Prof. Dan Chambers and Dr Simon Apte
Silicosis is now being viewed as the ‘new asbestosis’ affecting a new generation of people who have been exposed to high-silica products including the popular engineered stone products used in bench tops. At the moment silicosis cannot be cured. At best it is debilitating, and at its worst can be fatal. Thousands of tradespeople are at risk of this deadly disease. Hundreds have been diagnosed in Queensland alone.
Professor Dan Chambers and his team have found a way to treat those with early-stage silicosis called whole lung lavage and it involves washing the toxic silica crystals out of the lungs with 25 litres of warm saline solution.
The breakthrough came by being able to measure the amount of silica in the lungs of patients and gave our researchers the chance to measure the extent of the problem and gauge the potential success of this new treatment.
Using blood to help predict lung cancer progression
Professor Kwun Fong – Thoracic Physician and Head Pulmonary Malignancy Services at The Prince Charles Hospital
Currently, surgery is regarded as the best treatment for early stage lung cancer. However, people who have had surgery to remove a lung cancer tumour remain at risk of developing it again in the future.
This means patients who have lung cancer must undergo invasive biopsies of their lungs in order for the clinician to assess what treatment is needed, and the potential recurrence of the disease. However, around 20% of patients are unable to have their lung cancer biopsied due to other serious health conditions that make the biopsy procedure too risky.
Professor Kwun Fong and his team are committed to finding a way to non-invasively predict disease progression in lung cancer patients, by assessing their blood. Professor Kwun Fong and his team will test the “exosomal lung prognosticator (ELP)” panel, developed A/Prof Moller, on stored lung cancer tissue and blood samples to see if the progression of lung cancer in these patients was evident in these exosomes.
The success of this study could change the way lung cancer treatments are assessed and allow our most unwell patients to receive the treatments they so desperately need.
Stem cell therapy for lung disease
Professor Dan Chambers – Queensland Lung Transplant Service research laboratory.
Idiopathic pulmonary fibrosis (IPF) is a debilitating lung disease that affects more than 2,000 Australians. It attacks the tissue in the lungs, causing each lung to become stiff and making everyday tasks like walking up-stairs near impossible.
A life with IPF is short and painful, with most patients passing away only three to five years after their diagnosis. Patients are left breathless, tired and often with a constant dry cough. Unfortunately, there are virtually no options in the treatment of IPF other than making the patient as comfortable as possible.
That is why Professor Dan Chambers and his team in the thoracic lab at The Prince Charles Hospital are looking for the first key in effectively treating IPF. One of the characteristics of the disease is the apparent depletion of a certain type of stem cell in the lungs – mesenchymal stem cells (MSCs). Professor Chambers and his team are working hard to find out whether we can we simply replace the lost MSCs with new ones, and if that will improve the lives of IPF patients.
His study is already showing positive results, and if successful will not only help patients with IPF but could be the solution for other lung diseases and even lung transplant treatments.